InVivoMAb anti-mouse IFNγ
Product Details
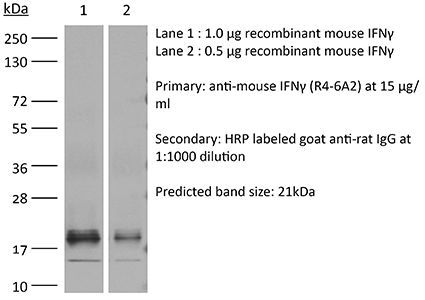
The R4-6A2 monoclonal antibody reacts with mouse IFNγ (interferon gamma) a 20 kDa soluble pleiotropic cytokine and the sole member of the type II class of interferons. IFNγ is primarily produced by activated lymphocytes including T, B, NK cells, and ILCs. IFNγ exerts immunoregulatory, anti-proliferative, anti-viral, and proinflammatory activities and plays an important role in activation, growth, and differentiation of T and B lymphocytes, macrophages, NK cells and other non-hematopoietic cell types. Additionally, IFNγ induces the production of cytokines, Fc receptor, and adhesion molecules and up-regulates MHC class I and II antigen expression by antigen presenting cells during an immune response. IFNγ has also been shown to modulate macrophage effector functions, influence isotype switching and induce the secretion of immunoglobulins by B cells. IFNγ signals through the IFN gamma receptor which exists as a heterodimer composed of CD119 (IFNγ receptor 1) and AF-1 (IFNγ receptor 2). The IFNγ receptor is expressed ubiquitously on almost all cell types with the exception of mature erythrocytes. The R4-6A2 antibody has been shown to neutralize both natural and recombinant IFNγ.Specifications
| Isotype | Rat IgG1, κ |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb rat IgG1 isotype control, anti-horseradish peroxidase |
| Recommended Dilution Buffer | InVivoPure pH 8.0 Dilution Buffer |
| Immunogen | Partially-purified native mouse IFNγ |
| Reported Applications |
in vivo IFNγ neutralization in vitro IFNγ neutralization |
| Formulation |
PBS, pH 8.0 Contains no stabilizers or preservatives |
| Endotoxin |
<2EU/mg (<0.002EU/μg) Determined by LAL gel clotting assay |
| Sterility | 0.2 µm filtration |
| Production | Purified from tissue culture supernatant in an animal free facility |
| Purification | Protein G |
| RRID | AB_1107692 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
Recommended Products
in vivo IFNγ neutralization
IFN-gamma dictates allograft fate via opposing effects on the graft and on recipient CD8 T cell responses PubMed
CD8 T cells are necessary for costimulation blockade-resistant rejection. However, the mechanism by which CD8 T cells mediate rejection in the absence of major costimulatory signals is poorly understood. IFN-gamma promotes CD8 T cell-mediated immune responses, but IFN-gamma-deficient mice show early graft loss despite costimulation blockade. In contrast, we found that IFN-gamma receptor knockout mice show dramatically prolonged graft survival under costimulation blockade. To investigate this paradox, we addressed the effects of IFN-gamma on T cell alloresponses in vivo independent of the effects of IFN-gamma on graft survival. We identified a donor-specific CD8 T cell breakthrough response temporally correlated with costimulation blockade-resistant rejection. Neither IFN-gamma receptor knockout recipients nor IFN-gamma-deficient recipients showed a CD8 breakthrough response. Graft death on IFN-gamma-deficient recipients despite costimulation blockade could be explained by the lack of IFN-gamma available to act on the graft. Indeed, the presence of IFN-gamma was necessary for graft survival on IFN-gamma receptor knockout recipients, as either IFN-gamma neutralization or the lack of the IFN-gamma receptor on the graft precipitated early graft loss. Thus, IFN-gamma is required both for the recipient to mount a donor-specific CD8 T cell response under costimulation blockade as well as for the graft to survive after allotransplantation.
in vitro IFNγ neutralization
In vivo induction of Tr1 cells via mucosal dendritic cells and AHR signaling PubMed
BACKGROUND: Type 1 regulatory T (Tr1) cells, characterized by the secretion of high levels of the anti-inflammatory cytokine interleukin-10 (IL-10), play an important role in the regulation of autoimmune diseases and transplantation. However, effective strategies that specifically induce Tr1 cells in vivo are limited. Furthermore, the pathways controlling the induction of these cells in vivo are not well understood. METHODOLOGY/PRINCIPAL FINDINGS: Here we report that nasal administration of anti-CD3 antibody induces suppressive Tr1 cells in mice. The in vivo induction of Tr1 cells by nasal anti-CD3 is dependent on IL-27 produced by upper airway resident dendritic cells (DCs), and is controlled by the transcription factors aryl hydrocarbon receptor (AHR) and c-Maf. Subsequently, IL-21 acts in an autocrine fashion to expand and maintain the Tr1 cells induced in vivo by nasally administered anti-CD3. CONCLUSIONS/SIGNIFICANCE: Our findings identify a unique approach to generate Tr1 cells in vivo and provide insights into the mechanisms by which these cells are induced.
in vivo IFNγ neutralization
Oncolytic adenovirus expressing IL-23 and p35 elicits IFN-gamma- and TNF-alpha-co-producing T cell-mediated antitumor immunity PubMed
Cytokine immunogene therapy is a promising strategy for cancer treatment. Interleukin (IL)-12 boosts potent antitumor immunity by inducing T helper 1 cell differentiation and stimulating cytotoxic T lymphocyte and natural killer cell cytotoxicity. IL-23 has been proposed to have similar but not overlapping functions with IL-12 in inducing Th1 cell differentiation and antitumor immunity. However, the therapeutic effects of intratumoral co-expression of IL-12 and IL-23 in a cancer model have yet to be investigated. Therefore, we investigated for the first time an effective cancer immunogene therapy of syngeneic tumors via intratumoral inoculation of oncolytic adenovirus co-expressing IL-23 and p35, RdB/IL23/p35. Intratumoral administration of RdB/IL23/p35 elicited strong antitumor effects and increased survival in a murine B16-F10 syngeneic tumor model. The levels of IL-12, IL-23, interferon-gamma (IFN-gamma), and tumor necrosis factor-alpha (TNF-alpha) were elevated in RdB/IL23/p35-treated tumors. Moreover, the proportion of regulatory T cells was markedly decreased in mice treated with RdB/IL23/p35. Consistent with these data, mice injected with RdB/IL23/p35 showed massive infiltration of CD4(+) and CD8(+) T cells into the tumor as well as enhanced induction of tumor-specific immunity. Importantly, therapeutic mechanism of antitumor immunity mediated by RdB/IL23/p35 is associated with the generation and recruitment of IFN-gamma- and TNF-alpha-co-producing T cells in tumor microenvironment. These results provide a new insight into therapeutic mechanisms of IL-12 plus IL-23 and provide a potential clinical cancer immunotherapeutic agent for improved antitumor immunity.
in vivo IFNγ neutralization, in vivo TNFα neutralization
Production and differentiation of myeloid cells driven by proinflammatory cytokines in response to acute pneumovirus infection in mice PubMed
Respiratory virus infections are often pathogenic, driving severe inflammatory responses. Most research has focused on localized effects of virus infection and inflammation. However, infection can induce broad-reaching, systemic changes that are only beginning to be characterized. In this study, we assessed the impact of acute pneumovirus infection in C57BL/6 mice on bone marrow hematopoiesis. We hypothesized that inflammatory cytokine production in the lung upregulates myeloid cell production in response to infection. We demonstrate a dramatic increase in the percentages of circulating myeloid cells, which is associated with pronounced elevations in inflammatory cytokines in serum (IFN-gamma, IL-6, CCL2), bone (TNF-alpha), and lung tissue (TNF-alpha, IFN-gamma, IL-6, CCL2, CCL3, G-CSF, osteopontin). Increased hematopoietic stem/progenitor cell percentages (Lineage(-)Sca-I(+)c-kit(+)) were also detected in the bone marrow. This increase was accompanied by an increase in the proportions of committed myeloid progenitors, as determined by colony-forming unit assays. However, no functional changes in hematopoietic stem cells occurred, as assessed by competitive bone marrow reconstitution. Systemic administration of neutralizing Abs to either TNF-alpha or IFN-gamma blocked expansion of myeloid progenitors in the bone marrow and also limited virus clearance from the lung. These findings suggest that acute inflammatory cytokines drive production and differentiation of myeloid cells in the bone marrow by inducing differentiation of committed myeloid progenitors. Our findings provide insight into the mechanisms via which innate immune responses regulate myeloid cell progenitor numbers in response to acute respiratory virus infection.
in vivo IFNγ neutralization, in vivo IL-6 neutralization, in vivo LFA-1 neutralization
Donor CD4 T cells trigger costimulation blockade-resistant donor bone marrow rejection through bystander activation requiring IL-6 PubMed
Bone marrow (BM) transplantation under costimulation blockade induces chimerism and tolerance. Cotransplantation of donor T cells (contained in substantial numbers in mobilized peripheral blood stem cells and donor lymphocyte infusions) together with donor BM paradoxically triggers rejection of donor BM through undefined mechanisms. Here, nonmyeloablatively irradiated C57BL/6 recipients simultaneously received donor BM (BALB/c) and donor T cells under costimulation blockade (anti-CD154 and CTLA4Ig). Donor CD4, but not CD8 cells, triggered natural killer-independent donor BM rejection which was associated with increased production of IL-6, interferon gamma (IFN-gamma) and IL-17A. BM rejection was prevented through neutralization of IL-6, but not of IFN-gamma or IL-17A. IL-6 counteracted the antiproliferative effect of anti-CD154 in vitro. Rapamycin and anti-lymphocyte function-associated antigen 1 negated this effect of IL-6 in vitro and prevented BM rejection in vivo. Simultaneous cotransplantation of (BALB/cxB6)F1, recipient or irradiated donor CD4 cells, or late transfer of donor CD4 cells did not lead to BM rejection, whereas cotransplantation of third party CD4 cells did. Transferred donor CD4 cells became activated, rapidly underwent apoptosis and triggered activation and proliferation of recipient T cells. Collectively, these results provide evidence that donor T cells recognizing the recipient as allogeneic lead to the release of IL-6, which abolishes the effect of anti-CD154, triggering donor BM rejection through bystander activation.
Flow Cytometry, in vivo CD8+ T cell depletion, in vivo IFNγ neutralization, in vivo NK cell depletion
Animal model of respiratory syncytial virus: CD8+ T cells cause a cytokine storm that is chemically tractable by sphingosine-1-phosphate 1 receptor agonist therapy PubMed
The cytokine storm is an intensified, dysregulated, tissue-injurious inflammatory response driven by cytokine and immune cell components. The cytokine storm during influenza virus infection, whereby the amplified innate immune response is primarily responsible for pulmonary damage, has been well characterized. Now we describe a novel event where virus-specific T cells induce a cytokine storm. The paramyxovirus pneumonia virus of mice (PVM) is a model of human respiratory syncytial virus (hRSV). Unexpectedly, when C57BL/6 mice were infected with PVM, the innate inflammatory response was undetectable until day 5 postinfection, at which time CD8(+) T cells infiltrated into the lung, initiating a cytokine storm by their production of gamma interferon (IFN-gamma) and tumor necrosis factor alpha (TNF-alpha). Administration of an immunomodulatory sphingosine-1-phosphate (S1P) receptor 1 (S1P1R) agonist significantly inhibited PVM-elicited cytokine storm by blunting the PVM-specific CD8(+) T cell response, resulting in diminished pulmonary disease and enhanced survival. IMPORTANCE: A dysregulated overly exuberant immune response, termed a “cytokine storm,” accompanies virus-induced acute respiratory diseases (VARV), is primarily responsible for the accompanying high morbidity and mortality, and can be controlled therapeutically in influenza virus infection of mice and ferrets by administration of sphingosine-1-phosphate 1 receptor (S1P1R) agonists. Here, two novel findings are recorded. First, in contrast to influenza infection, where the cytokine storm is initiated early by the innate immune system, for pneumonia virus of mice (PVM), a model of RSV, the cytokine storm is initiated late in infection by the adaptive immune response: specifically, by virus-specific CD8 T cells via their release of IFN-gamma and TNF-alpha. Blockading these cytokines with neutralizing antibodies blunts the cytokine storm and protects the host. Second, PVM infection is controlled by administration of an S1P1R agonist.
Flow Cytometry, in vitro IFNγ neutralization, in vivo CD4+ T cell depletion, in vivo CD8+ T cell depletion, in vivo NK cell depletion
NK cells link obesity-induced adipose stress to inflammation and insulin resistance PubMed
An important cause of obesity-induced insulin resistance is chronic systemic inflammation originating in visceral adipose tissue (VAT). VAT inflammation is associated with the accumulation of proinflammatory macrophages in adipose tissue, but the immunological signals that trigger their accumulation remain unknown. We found that a phenotypically distinct population of tissue-resident natural killer (NK) cells represented a crucial link between obesity-induced adipose stress and VAT inflammation. Obesity drove the upregulation of ligands of the NK cell-activating receptor NCR1 on adipocytes; this stimulated NK cell proliferation and interferon-gamma (IFN-gamma) production, which in turn triggered the differentiation of proinflammatory macrophages and promoted insulin resistance. Deficiency of NK cells, NCR1 or IFN-gamma prevented the accumulation of proinflammatory macrophages in VAT and greatly ameliorated insulin sensitivity. Thus NK cells are key regulators of macrophage polarization and insulin resistance in response to obesity-induced adipocyte stress.
in vivo blocking of CD40/CD40L signaling, in vivo CD40 activation, in vivo CSF1 neutralization, in vivo IFNγ neutralization, in vivo neutrophil depletion
DC-SIGN(+) Macrophages Control the Induction of Transplantation Tolerance PubMed
Tissue effector cells of the monocyte lineage can differentiate into different cell types with specific cell function depending on their environment. The phenotype, developmental requirements, and functional mechanisms of immune protective macrophages that mediate the induction of transplantation tolerance remain elusive. Here, we demonstrate that costimulatory blockade favored accumulation of DC-SIGN-expressing macrophages that inhibited CD8(+) T cell immunity and promoted CD4(+)Foxp3(+) Treg cell expansion in numbers. Mechanistically, that simultaneous DC-SIGN engagement by fucosylated ligands and TLR4 signaling was required for production of immunoregulatory IL-10 associated with prolonged allograft survival. Deletion of DC-SIGN-expressing macrophages in vivo, interfering with their CSF1-dependent development, or preventing the DC-SIGN signaling pathway abrogated tolerance. Together, the results provide new insights into the tolerogenic effects of costimulatory blockade and identify DC-SIGN(+) suppressive macrophages as crucial mediators of immunological tolerance with the concomitant therapeutic implications in the clinic.
Flow Cytometry, in vivo IFNγ neutralization, in vivo IL-12 neutralization, in vivo regulatory T cell depletion
Anti-CD20 therapy induces a memory Th1 response through the IFN-gamma/IL-12 axis and prevents protumor regulatory T-cell expansion in mice PubMed
The long-lasting clinical response by lymphoma patients to anti-CD20 therapy has been attributed to the induction of an anti-tumor adaptive immunity. We previously demonstrated that a CD4-dependent mechanism is responsible for the long-term protection of CD20(+) tumor-bearing mice by anti-CD20 treatment. Here, we compare tumor immunity in tumor-bearing animals that did or did not receive anti-CD20 treatment. Splenic CD4(+)FoxP3(+) regulatory T cells (Tregs) expanded substantially in untreated mice that exhibited then a reduced survival, whereas Tregs depletion led to long-term survival of the animals, suggesting the establishment of a Treg-dependent immunosuppressive environment after tumor injection. Strikingly, anti-CD20 therapy reversed the initial expansion of Tregs, and was accompanied by a marked increase in the number of Th1 cells, with no detectable change in Th2 and Th17 cell numbers. Interleukin-12 serum level was also increased by the anti-CD20 treatment, and activated myeloid dendritic cells producing interleukin-12 could be detected in lymph nodes of treated animals, while interferon-gamma blockade strongly reduced survival. Also, CD4(+) effector memory T cells were evidenced in surviving animals, and the transfer of CD4(+) T cells induced long-term protection. Thus, anti-CD20 therapy promotes strong anti-tumor adaptive immunity, opposes Treg expansion and inhibits tumor cells from maintaining an immunosuppressive environment.
in vivo IFNγ neutralization, in vivo IL-10 neutralization, in vivo IL-21R blockade, in vivo regulatory T cell depletion, in vivo TGFβ neutralization
Expanding antigen-specific regulatory networks to treat autoimmunity PubMed
Regulatory T cells hold promise as targets for therapeutic intervention in autoimmunity, but approaches capable of expanding antigen-specific regulatory T cells in vivo are currently not available. Here we show that systemic delivery of nanoparticles coated with autoimmune-disease-relevant peptides bound to major histocompatibility complex class II (pMHCII) molecules triggers the generation and expansion of antigen-specific regulatory CD4(+) T cell type 1 (TR1)-like cells in different mouse models, including mice humanized with lymphocytes from patients, leading to resolution of established autoimmune phenomena. Ten pMHCII-based nanomedicines show similar biological effects, regardless of genetic background, prevalence of the cognate T-cell population or MHC restriction. These nanomedicines promote the differentiation of disease-primed autoreactive T cells into TR1-like cells, which in turn suppress autoantigen-loaded antigen-presenting cells and drive the differentiation of cognate B cells into disease-suppressing regulatory B cells, without compromising systemic immunity. pMHCII-based nanomedicines thus represent a new class of drugs, potentially useful for treating a broad spectrum of autoimmune conditions in a disease-specific manner.