InVivoMAb anti-human/monkey CD28
Product Description
Specifications
| Isotype | Mouse IgG1, κ |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb mouse IgG1 isotype control, unknown specificity |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Human CD28 transfected cell line |
| Reported Applications |
in vitro T cell stimulation/activation Immunoprecipitation Flow cytometry Immunohistochemistry (frozen) |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
≤1EU/mg (≤0.001EU/μg) Determined by LAL assay |
| Purity |
≥95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| RRID | AB_2687814 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
| Need a Custom Formulation? | See All Antibody Customization Options |
Application References
in vitro T cell stimulation/activation
Blewett, M. M., et al (2016). "Chemical proteomic map of dimethyl fumarate-sensitive cysteines in primary human T cells" Sci Signal 9(445): rs10.
PubMed
Dimethyl fumarate (DMF) is an electrophilic drug that is used to treat autoimmune conditions, including multiple sclerosis and psoriasis. The mechanism of action of DMF is unclear but may involve the covalent modification of proteins or DMF serving as a prodrug that is converted to monomethyl fumarate (MMF). We found that DMF, but not MMF, blocked the activation of primary human and mouse T cells. Using a quantitative, site-specific chemical proteomic platform, we determined the DMF sensitivity of >2400 cysteine residues in human T cells. Cysteines sensitive to DMF, but not MMF, were identified in several proteins with established biochemical or genetic links to T cell function, including protein kinase Ctheta (PKCtheta). DMF blocked the association of PKCtheta with the costimulatory receptor CD28 by perturbing a CXXC motif in the C2 domain of this kinase. Mutation of these DMF-sensitive cysteines also impaired PKCtheta-CD28 interactions and T cell activation, designating the C2 domain of PKCtheta as a key functional, electrophile-sensing module important for T cell biology.
Immunohistochemistry (frozen)
Battifora, M., et al (1998). "B7.1 costimulatory molecule is expressed on thyroid follicular cells in Hashimoto’s thyroiditis, but not in Graves’ disease" J Clin Endocrinol Metab 83(11): 4130-4139.
PubMed
The molecules of the B7 family play a major role in T-lymphocyte costimulation through interaction with their counterreceptors CD28 and CTLA4. In the present study, we analyzed the possible expression of B7 molecules on surgically removed thyroid tissue of patients with autoimmune [Hashimoto’s thyroiditis (HT) or Graves’ disease (GD)] or nonautoimmune [nontoxic goiter (NTG) or papillary cancer (PC)] thyroid diseases. We found clear positivity of thyroid follicular cells for B7.1 in HT but not in GD, nor in nonautoimmune specimens (NTG, PC) using in situ analysis by alkaline phosphatase anti-alkaline phosphatase (APAAP) technique. Double immunostaining experiments in combination with an anti-human thyroglobulin antibody confirmed follicular B7.1 localization. On the contrary, no follicular B7.2 expression was observed in any specimen analyzed. These findings were confirmed by immunofluorescence flow cytometry on isolated follicular cells. The cytokines IL1beta and LPS were able to induce de novo B7.1 expression on cultured thyroid follicular cells. Intrathyroid T cells proved responsive to stimulation via the B7 ligand CD28, even in the absence of IL2. Moreover preliminary evidence was obtained for an inhibitory effect of anti-B7.1 mAb on T-cell proliferation in coculture with isolated thyroid follicular cells. It is conceivable that in HT, expression of B7.1 on follicular cells, together with MHC class II antigens and ICAM1, could provide a local costimulatory signal for T-lymphocyte differentiation toward the type 1 cytokine secretion pattern and maintenance of the autoimmune process.
Immunohistochemistry (frozen)
Tazi, A., et al (1999). "Evidence that Langerhans cells in adult pulmonary Langerhans cell histiocytosis are mature dendritic cells: importance of the cytokine microenvironment" J Immunol 163(6): 3511-3515.
PubMed
Because Langerhans cells (LC) in peripheral tissues are generally “immature” cells with poor lymphostimulatory activity, the contribution of immune responses initiated by LC to the pathogenesis of pulmonary LC histiocytosis (LCH) has been uncertain. In this study we demonstrate that LC accumulating in LCH granulomas are phenotypically similar to mature lymphostimulatory dendritic cells present in lymphoid organs. LC in LCH granulomas intensely expressed B7-1 and B7-2 molecules, whereas normal pulmonary LC and LC accumulating in other pathologic lung disorders did not express these costimulatory molecules. The presence of B7+ LC in LCH granulomas was associated with the expression in these lesions, but not at other sites in the lung, of a unique profile of cytokines (presence of GM-CSF, TNF-alpha, and IL-1beta and the absence of IL-10) that is known to promote the in vitro differentiation of LC into cells expressing a lymphostimulatory phenotype. Finally, LCH granulomas were the only site where CD154-positive T cells could be identified in close contact with LC intensely expressing CD40 Ags. Taken together, these results strongly support the idea that an abnormal immune response initiated by LC may participate in the pathogenesis of pulmonary LCH, and suggest that therapeutic strategies aimed at modifying the lymphostimulatory phenotype of LC may be useful in the treatment of this disorder.
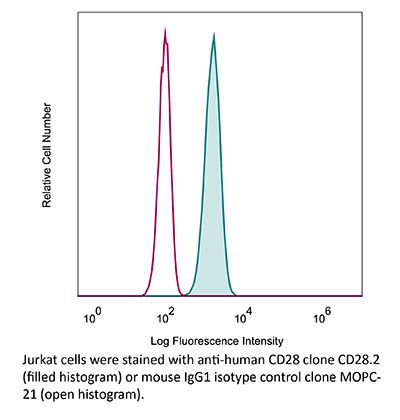
Flow Cytometry
Rout, N., et al (2010). "Paucity of CD4+ natural killer T (NKT) lymphocytes in sooty mangabeys is associated with lack of NKT cell depletion after SIV infection" PLoS One 5(3): e9787.
PubMed
Lack of chronic immune activation in the presence of persistent viremia is a key feature that distinguishes nonpathogenic simian immunodeficiency virus (SIV) infection in natural hosts from pathogenic SIV and HIV infection. To elucidate novel mechanisms downmodulating immune activation in natural hosts of SIV infection, we investigated natural killer T (NKT) lymphocytes in sooty mangabeys. NKT lymphocytes are a potent immunoregulatory arm of the innate immune system that recognize glycolipid antigens presented on the nonpolymorphic MHC-class I-like CD1d molecules. In a cross-sectional analysis of 50 SIV-negative and 50 naturally SIV-infected sooty mangabeys, ligand alpha-galactosylceramide loaded CD1d tetramers co-staining with Valpha24-positive invariant NKT lymphocytes were detected at frequencies >or=0.002% of circulating T lymphocytes in approximately half of the animals. In contrast to published reports in Asian macaques, sooty mangabey NKT lymphocytes consisted of CD8(+) and CD4/CD8 double-negative T lymphocytes that were CXCR3-positive and CCR5-negative suggesting that they trafficked to sites of inflammation without being susceptible to SIV infection. Consistent with these findings, there was no difference in the frequency or phenotype of NKT lymphocytes between SIV-negative and SIV-infected sooty mangabeys. On stimulation with alpha-galactosylceramide loaded on human CD1d molecules, sooty mangabey NKT lymphocytes underwent degranulation and secreted IFN-gamma, TNF-alpha, IL-2, IL-13, and IL-10, indicating the presence of both effector and immunoregulatory functional capabilities. The unique absence of CD4(+) NKT lymphocytes in sooty mangabeys, combined with their IL-10 cytokine-secreting ability and preservation following SIV infection, raises the possibility that NKT lymphocytes might play a role in downmodulating immune activation in SIV-infected sooty mangabeys.
Flow Cytometry
Leonard, J. A., et al (2011). "HIV-1 Nef disrupts intracellular trafficking of major histocompatibility complex class I, CD4, CD8, and CD28 by distinct pathways that share common elements" J Virol 85(14): 6867-6881.
PubMed
The Nef protein is an important HIV virulence factor that promotes the degradation of host proteins to augment virus production and facilitate immune evasion. The best-characterized targets of Nef are major histocompatibility complex class I (MHC-I) and CD4, but Nef also has been reported to target several other proteins, including CD8beta, CD28, CD80, CD86, and CD1d. To compare and contrast the effects of Nef on each protein, we constructed a panel of chimeric proteins in which the extracellular and transmembrane regions of the MHC-I allele HLA-A2 were fused to the cytoplasmic tails of CD4, CD28, CD8beta, CD80, CD86, and CD1d. We found that Nef coprecipitated with and disrupted the expression of molecules with cytoplasmic tails from MHC-I HLA-A2, CD4, CD8beta, and CD28, but Nef did not bind to or alter the expression of molecules with cytoplasmic tails from CD80, CD86, and CD1d. In addition, we used short interfering RNA (siRNA) knockdown and coprecipitation experiments to implicate AP-1 as a cellular cofactor for Nef in the downmodulation of both CD28 and CD8beta. The interaction with AP-1 required for CD28 and CD8beta differed from the AP-1 interaction required for MHC-I downmodulation in that it was mediated through the dileucine motif within Nef (LL(164,165)AA) and did not require the tyrosine binding pocket of the AP-1 mu subunit. In addition, we demonstrate a requirement for beta-COP as a cellular cofactor for Nef that was necessary for the degradation of targeted molecules HLA-A2, CD4, and CD8. These studies provide important new information on the similarities and differences with which Nef affects intracellular trafficking and help focus future research on the best potential pharmaceutical targets.
in vitro T cell stimulation/activation
Oh, Y. M., et al (2015). "Ndrg1 is a T-cell clonal anergy factor negatively regulated by CD28 costimulation and interleukin-2" Nat Commun 6: 8698.
PubMed
Induction of T-cell clonal anergy involves serial activation of transcription factors, including NFAT and Egr2/3. However, downstream effector mechanisms of these transcription factors are not fully understood yet. Here we identify Ndrg1 as an anergy factor induced by Egr2. Ndrg1 is upregulated by anergic signalling and maintained at high levels in resting anergic T cells. Overexpression of Ndrg1 mimics the anergic state and knockout of the gene prevents anergy induction. Interestingly, Ndrg1 is phosphorylated and degraded by CD28 signalling in a proteasome-dependent manner, explaining the costimulation dependence of anergy prevention. Similarly, IL-2 treatment of anergic T cells, under conditions that lead to the reversal of anergy, also induces Ndrg1 phosphorylation and degradation. Finally, older Ndrg1-deficient mice show T-cell hyperresponsiveness and Ndrg1-deficient T cells aggravate inducible autoimmune inflammation. Thus, Ndrg1 contributes to the maintenance of clonal anergy and inhibition of T-cell-mediated inflammation.
in vitro T cell stimulation/activation
Edwards, L. J., et al (2015). "Signal transducer and activator of transcription (STAT) 3 inhibition delays the onset of lupus nephritis in MRL/lpr mice" Clin Immunol 158(2): 221-230.
PubMed
The transcription factor STAT3 is overexpressed and hyperactivated in T cells from SLE patients. STAT3 plays a central role in T cell differentiation into Th17 and T follicular helper cells, two subsets that orchestrate autoimmune responses in SLE. Moreover, STAT3 is important in chemokine-mediated T cell migration. To better understand its role in SLE, we inhibited STAT3 in lupus-prone mice using the small molecule Stattic. Stattic-treated mice exhibited delayed onset of proteinuria (3 weeks later than controls), and had lower levels of anti-dsDNA antibodies and inflammatory cytokines. Inhibitor treatment reduced lymphadenopathy, resulted in a 3-fold decrease in total T cell number, and a 4-fold decrease in the numbers of T follicular helper cells. In vitro experiments showed that Stattic-treated T cells exhibited decreased proliferation and a decrease in ability to migrate to CXCL12. We propose that STAT3 inhibition represents a therapeutic target in SLE, particularly lupus nephritis.
in vitro T cell stimulation/activation
Blewett, M. M., et al (2016). "Chemical proteomic map of dimethyl fumarate-sensitive cysteines in primary human T cells" Sci Signal 9(445): rs10.
PubMed
Dimethyl fumarate (DMF) is an electrophilic drug that is used to treat autoimmune conditions, including multiple sclerosis and psoriasis. The mechanism of action of DMF is unclear but may involve the covalent modification of proteins or DMF serving as a prodrug that is converted to monomethyl fumarate (MMF). We found that DMF, but not MMF, blocked the activation of primary human and mouse T cells. Using a quantitative, site-specific chemical proteomic platform, we determined the DMF sensitivity of >2400 cysteine residues in human T cells. Cysteines sensitive to DMF, but not MMF, were identified in several proteins with established biochemical or genetic links to T cell function, including protein kinase Ctheta (PKCtheta). DMF blocked the association of PKCtheta with the costimulatory receptor CD28 by perturbing a CXXC motif in the C2 domain of this kinase. Mutation of these DMF-sensitive cysteines also impaired PKCtheta-CD28 interactions and T cell activation, designating the C2 domain of PKCtheta as a key functional, electrophile-sensing module important for T cell biology.
Immunoprecipitation
Zhao, Y., et al (2019). "PD-L1:CD80 Cis-Heterodimer Triggers the Co-stimulatory Receptor CD28 While Repressing the Inhibitory PD-1 and CTLA-4 Pathways" Immunity 51(6): 1059-1073.e1059.
PubMed
Combined immunotherapy targeting the immune checkpoint receptors cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) and programmed cell death 1 (PD-1), or CTLA-4 and the PD-1 ligand (PD-L1) exhibits superior anti-tumor responses compared with single-agent therapy. Here, we examined the molecular basis for this synergy. Using reconstitution assays with fluorescence readouts, we found that PD-L1 and the CTLA-4 ligand CD80 heterodimerize in cis but not trans. Quantitative biochemistry and cell biology assays revealed that PD-L1:CD80 cis-heterodimerization inhibited both PD-L1:PD-1 and CD80:CTLA-4 interactions through distinct mechanisms but preserved the ability of CD80 to activate the T cell co-stimulatory receptor CD28. Furthermore, PD-L1 expression on antigen-presenting cells (APCs) prevented CTLA-4-mediated trans-endocytosis of CD80. Atezolizumab (anti-PD-L1), but not anti-PD-1, reduced cell surface expression of CD80 on APCs, and this effect was negated by co-blockade of CTLA-4 with ipilimumab (anti-CTLA-4). Thus, PD-L1 exerts an immunostimulatory effect by repressing the CTLA-4 axis; this has implications to the synergy of anti-PD-L1 and anti-CTLA-4 combination therapy.
Immunohistochemistry (frozen)
Battifora, M., et al (1998). "B7.1 costimulatory molecule is expressed on thyroid follicular cells in Hashimoto’s thyroiditis, but not in Graves’ disease" J Clin Endocrinol Metab 83(11): 4130-4139.
PubMed
The molecules of the B7 family play a major role in T-lymphocyte costimulation through interaction with their counterreceptors CD28 and CTLA4. In the present study, we analyzed the possible expression of B7 molecules on surgically removed thyroid tissue of patients with autoimmune [Hashimoto’s thyroiditis (HT) or Graves’ disease (GD)] or nonautoimmune [nontoxic goiter (NTG) or papillary cancer (PC)] thyroid diseases. We found clear positivity of thyroid follicular cells for B7.1 in HT but not in GD, nor in nonautoimmune specimens (NTG, PC) using in situ analysis by alkaline phosphatase anti-alkaline phosphatase (APAAP) technique. Double immunostaining experiments in combination with an anti-human thyroglobulin antibody confirmed follicular B7.1 localization. On the contrary, no follicular B7.2 expression was observed in any specimen analyzed. These findings were confirmed by immunofluorescence flow cytometry on isolated follicular cells. The cytokines IL1beta and LPS were able to induce de novo B7.1 expression on cultured thyroid follicular cells. Intrathyroid T cells proved responsive to stimulation via the B7 ligand CD28, even in the absence of IL2. Moreover preliminary evidence was obtained for an inhibitory effect of anti-B7.1 mAb on T-cell proliferation in coculture with isolated thyroid follicular cells. It is conceivable that in HT, expression of B7.1 on follicular cells, together with MHC class II antigens and ICAM1, could provide a local costimulatory signal for T-lymphocyte differentiation toward the type 1 cytokine secretion pattern and maintenance of the autoimmune process.
Immunohistochemistry (frozen)
Tazi, A., et al (1999). "Evidence that Langerhans cells in adult pulmonary Langerhans cell histiocytosis are mature dendritic cells: importance of the cytokine microenvironment" J Immunol 163(6): 3511-3515.
PubMed
Because Langerhans cells (LC) in peripheral tissues are generally “immature” cells with poor lymphostimulatory activity, the contribution of immune responses initiated by LC to the pathogenesis of pulmonary LC histiocytosis (LCH) has been uncertain. In this study we demonstrate that LC accumulating in LCH granulomas are phenotypically similar to mature lymphostimulatory dendritic cells present in lymphoid organs. LC in LCH granulomas intensely expressed B7-1 and B7-2 molecules, whereas normal pulmonary LC and LC accumulating in other pathologic lung disorders did not express these costimulatory molecules. The presence of B7+ LC in LCH granulomas was associated with the expression in these lesions, but not at other sites in the lung, of a unique profile of cytokines (presence of GM-CSF, TNF-alpha, and IL-1beta and the absence of IL-10) that is known to promote the in vitro differentiation of LC into cells expressing a lymphostimulatory phenotype. Finally, LCH granulomas were the only site where CD154-positive T cells could be identified in close contact with LC intensely expressing CD40 Ags. Taken together, these results strongly support the idea that an abnormal immune response initiated by LC may participate in the pathogenesis of pulmonary LCH, and suggest that therapeutic strategies aimed at modifying the lymphostimulatory phenotype of LC may be useful in the treatment of this disorder.
Flow Cytometry
Rout, N., et al (2010). "Paucity of CD4+ natural killer T (NKT) lymphocytes in sooty mangabeys is associated with lack of NKT cell depletion after SIV infection" PLoS One 5(3): e9787.
PubMed
Lack of chronic immune activation in the presence of persistent viremia is a key feature that distinguishes nonpathogenic simian immunodeficiency virus (SIV) infection in natural hosts from pathogenic SIV and HIV infection. To elucidate novel mechanisms downmodulating immune activation in natural hosts of SIV infection, we investigated natural killer T (NKT) lymphocytes in sooty mangabeys. NKT lymphocytes are a potent immunoregulatory arm of the innate immune system that recognize glycolipid antigens presented on the nonpolymorphic MHC-class I-like CD1d molecules. In a cross-sectional analysis of 50 SIV-negative and 50 naturally SIV-infected sooty mangabeys, ligand alpha-galactosylceramide loaded CD1d tetramers co-staining with Valpha24-positive invariant NKT lymphocytes were detected at frequencies >or=0.002% of circulating T lymphocytes in approximately half of the animals. In contrast to published reports in Asian macaques, sooty mangabey NKT lymphocytes consisted of CD8(+) and CD4/CD8 double-negative T lymphocytes that were CXCR3-positive and CCR5-negative suggesting that they trafficked to sites of inflammation without being susceptible to SIV infection. Consistent with these findings, there was no difference in the frequency or phenotype of NKT lymphocytes between SIV-negative and SIV-infected sooty mangabeys. On stimulation with alpha-galactosylceramide loaded on human CD1d molecules, sooty mangabey NKT lymphocytes underwent degranulation and secreted IFN-gamma, TNF-alpha, IL-2, IL-13, and IL-10, indicating the presence of both effector and immunoregulatory functional capabilities. The unique absence of CD4(+) NKT lymphocytes in sooty mangabeys, combined with their IL-10 cytokine-secreting ability and preservation following SIV infection, raises the possibility that NKT lymphocytes might play a role in downmodulating immune activation in SIV-infected sooty mangabeys.
in vitro T cell stimulation/activation
Oh, Y. M., et al (2015). "Ndrg1 is a T-cell clonal anergy factor negatively regulated by CD28 costimulation and interleukin-2" Nat Commun 6: 8698.
PubMed
Induction of T-cell clonal anergy involves serial activation of transcription factors, including NFAT and Egr2/3. However, downstream effector mechanisms of these transcription factors are not fully understood yet. Here we identify Ndrg1 as an anergy factor induced by Egr2. Ndrg1 is upregulated by anergic signalling and maintained at high levels in resting anergic T cells. Overexpression of Ndrg1 mimics the anergic state and knockout of the gene prevents anergy induction. Interestingly, Ndrg1 is phosphorylated and degraded by CD28 signalling in a proteasome-dependent manner, explaining the costimulation dependence of anergy prevention. Similarly, IL-2 treatment of anergic T cells, under conditions that lead to the reversal of anergy, also induces Ndrg1 phosphorylation and degradation. Finally, older Ndrg1-deficient mice show T-cell hyperresponsiveness and Ndrg1-deficient T cells aggravate inducible autoimmune inflammation. Thus, Ndrg1 contributes to the maintenance of clonal anergy and inhibition of T-cell-mediated inflammation.
Immunoprecipitation
Zhao, Y., et al (2019). "PD-L1:CD80 Cis-Heterodimer Triggers the Co-stimulatory Receptor CD28 While Repressing the Inhibitory PD-1 and CTLA-4 Pathways" Immunity 51(6): 1059-1073.e1059.
PubMed
Combined immunotherapy targeting the immune checkpoint receptors cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) and programmed cell death 1 (PD-1), or CTLA-4 and the PD-1 ligand (PD-L1) exhibits superior anti-tumor responses compared with single-agent therapy. Here, we examined the molecular basis for this synergy. Using reconstitution assays with fluorescence readouts, we found that PD-L1 and the CTLA-4 ligand CD80 heterodimerize in cis but not trans. Quantitative biochemistry and cell biology assays revealed that PD-L1:CD80 cis-heterodimerization inhibited both PD-L1:PD-1 and CD80:CTLA-4 interactions through distinct mechanisms but preserved the ability of CD80 to activate the T cell co-stimulatory receptor CD28. Furthermore, PD-L1 expression on antigen-presenting cells (APCs) prevented CTLA-4-mediated trans-endocytosis of CD80. Atezolizumab (anti-PD-L1), but not anti-PD-1, reduced cell surface expression of CD80 on APCs, and this effect was negated by co-blockade of CTLA-4 with ipilimumab (anti-CTLA-4). Thus, PD-L1 exerts an immunostimulatory effect by repressing the CTLA-4 axis; this has implications to the synergy of anti-PD-L1 and anti-CTLA-4 combination therapy.
in vitro T cell stimulation/activation
Edwards, L. J., et al (2015). "Signal transducer and activator of transcription (STAT) 3 inhibition delays the onset of lupus nephritis in MRL/lpr mice" Clin Immunol 158(2): 221-230.
PubMed
The transcription factor STAT3 is overexpressed and hyperactivated in T cells from SLE patients. STAT3 plays a central role in T cell differentiation into Th17 and T follicular helper cells, two subsets that orchestrate autoimmune responses in SLE. Moreover, STAT3 is important in chemokine-mediated T cell migration. To better understand its role in SLE, we inhibited STAT3 in lupus-prone mice using the small molecule Stattic. Stattic-treated mice exhibited delayed onset of proteinuria (3 weeks later than controls), and had lower levels of anti-dsDNA antibodies and inflammatory cytokines. Inhibitor treatment reduced lymphadenopathy, resulted in a 3-fold decrease in total T cell number, and a 4-fold decrease in the numbers of T follicular helper cells. In vitro experiments showed that Stattic-treated T cells exhibited decreased proliferation and a decrease in ability to migrate to CXCL12. We propose that STAT3 inhibition represents a therapeutic target in SLE, particularly lupus nephritis.
in vitro T cell stimulation/activation
Oh, Y. M., et al (2015). "Ndrg1 is a T-cell clonal anergy factor negatively regulated by CD28 costimulation and interleukin-2" Nat Commun 6: 8698.
PubMed
Induction of T-cell clonal anergy involves serial activation of transcription factors, including NFAT and Egr2/3. However, downstream effector mechanisms of these transcription factors are not fully understood yet. Here we identify Ndrg1 as an anergy factor induced by Egr2. Ndrg1 is upregulated by anergic signalling and maintained at high levels in resting anergic T cells. Overexpression of Ndrg1 mimics the anergic state and knockout of the gene prevents anergy induction. Interestingly, Ndrg1 is phosphorylated and degraded by CD28 signalling in a proteasome-dependent manner, explaining the costimulation dependence of anergy prevention. Similarly, IL-2 treatment of anergic T cells, under conditions that lead to the reversal of anergy, also induces Ndrg1 phosphorylation and degradation. Finally, older Ndrg1-deficient mice show T-cell hyperresponsiveness and Ndrg1-deficient T cells aggravate inducible autoimmune inflammation. Thus, Ndrg1 contributes to the maintenance of clonal anergy and inhibition of T-cell-mediated inflammation.
Flow Cytometry
Leonard, J. A., et al (2011). "HIV-1 Nef disrupts intracellular trafficking of major histocompatibility complex class I, CD4, CD8, and CD28 by distinct pathways that share common elements" J Virol 85(14): 6867-6881.
PubMed
The Nef protein is an important HIV virulence factor that promotes the degradation of host proteins to augment virus production and facilitate immune evasion. The best-characterized targets of Nef are major histocompatibility complex class I (MHC-I) and CD4, but Nef also has been reported to target several other proteins, including CD8beta, CD28, CD80, CD86, and CD1d. To compare and contrast the effects of Nef on each protein, we constructed a panel of chimeric proteins in which the extracellular and transmembrane regions of the MHC-I allele HLA-A2 were fused to the cytoplasmic tails of CD4, CD28, CD8beta, CD80, CD86, and CD1d. We found that Nef coprecipitated with and disrupted the expression of molecules with cytoplasmic tails from MHC-I HLA-A2, CD4, CD8beta, and CD28, but Nef did not bind to or alter the expression of molecules with cytoplasmic tails from CD80, CD86, and CD1d. In addition, we used short interfering RNA (siRNA) knockdown and coprecipitation experiments to implicate AP-1 as a cellular cofactor for Nef in the downmodulation of both CD28 and CD8beta. The interaction with AP-1 required for CD28 and CD8beta differed from the AP-1 interaction required for MHC-I downmodulation in that it was mediated through the dileucine motif within Nef (LL(164,165)AA) and did not require the tyrosine binding pocket of the AP-1 mu subunit. In addition, we demonstrate a requirement for beta-COP as a cellular cofactor for Nef that was necessary for the degradation of targeted molecules HLA-A2, CD4, and CD8. These studies provide important new information on the similarities and differences with which Nef affects intracellular trafficking and help focus future research on the best potential pharmaceutical targets.
Flow Cytometry
Rout, N., et al (2010). "Paucity of CD4+ natural killer T (NKT) lymphocytes in sooty mangabeys is associated with lack of NKT cell depletion after SIV infection" PLoS One 5(3): e9787.
PubMed
Lack of chronic immune activation in the presence of persistent viremia is a key feature that distinguishes nonpathogenic simian immunodeficiency virus (SIV) infection in natural hosts from pathogenic SIV and HIV infection. To elucidate novel mechanisms downmodulating immune activation in natural hosts of SIV infection, we investigated natural killer T (NKT) lymphocytes in sooty mangabeys. NKT lymphocytes are a potent immunoregulatory arm of the innate immune system that recognize glycolipid antigens presented on the nonpolymorphic MHC-class I-like CD1d molecules. In a cross-sectional analysis of 50 SIV-negative and 50 naturally SIV-infected sooty mangabeys, ligand alpha-galactosylceramide loaded CD1d tetramers co-staining with Valpha24-positive invariant NKT lymphocytes were detected at frequencies >or=0.002% of circulating T lymphocytes in approximately half of the animals. In contrast to published reports in Asian macaques, sooty mangabey NKT lymphocytes consisted of CD8(+) and CD4/CD8 double-negative T lymphocytes that were CXCR3-positive and CCR5-negative suggesting that they trafficked to sites of inflammation without being susceptible to SIV infection. Consistent with these findings, there was no difference in the frequency or phenotype of NKT lymphocytes between SIV-negative and SIV-infected sooty mangabeys. On stimulation with alpha-galactosylceramide loaded on human CD1d molecules, sooty mangabey NKT lymphocytes underwent degranulation and secreted IFN-gamma, TNF-alpha, IL-2, IL-13, and IL-10, indicating the presence of both effector and immunoregulatory functional capabilities. The unique absence of CD4(+) NKT lymphocytes in sooty mangabeys, combined with their IL-10 cytokine-secreting ability and preservation following SIV infection, raises the possibility that NKT lymphocytes might play a role in downmodulating immune activation in SIV-infected sooty mangabeys.
Immunohistochemistry (frozen)
Tazi, A., et al (1999). "Evidence that Langerhans cells in adult pulmonary Langerhans cell histiocytosis are mature dendritic cells: importance of the cytokine microenvironment" J Immunol 163(6): 3511-3515.
PubMed
Because Langerhans cells (LC) in peripheral tissues are generally “immature” cells with poor lymphostimulatory activity, the contribution of immune responses initiated by LC to the pathogenesis of pulmonary LC histiocytosis (LCH) has been uncertain. In this study we demonstrate that LC accumulating in LCH granulomas are phenotypically similar to mature lymphostimulatory dendritic cells present in lymphoid organs. LC in LCH granulomas intensely expressed B7-1 and B7-2 molecules, whereas normal pulmonary LC and LC accumulating in other pathologic lung disorders did not express these costimulatory molecules. The presence of B7+ LC in LCH granulomas was associated with the expression in these lesions, but not at other sites in the lung, of a unique profile of cytokines (presence of GM-CSF, TNF-alpha, and IL-1beta and the absence of IL-10) that is known to promote the in vitro differentiation of LC into cells expressing a lymphostimulatory phenotype. Finally, LCH granulomas were the only site where CD154-positive T cells could be identified in close contact with LC intensely expressing CD40 Ags. Taken together, these results strongly support the idea that an abnormal immune response initiated by LC may participate in the pathogenesis of pulmonary LCH, and suggest that therapeutic strategies aimed at modifying the lymphostimulatory phenotype of LC may be useful in the treatment of this disorder.
Immunohistochemistry (frozen)
Battifora, M., et al (1998). "B7.1 costimulatory molecule is expressed on thyroid follicular cells in Hashimoto’s thyroiditis, but not in Graves’ disease" J Clin Endocrinol Metab 83(11): 4130-4139.
PubMed
The molecules of the B7 family play a major role in T-lymphocyte costimulation through interaction with their counterreceptors CD28 and CTLA4. In the present study, we analyzed the possible expression of B7 molecules on surgically removed thyroid tissue of patients with autoimmune [Hashimoto’s thyroiditis (HT) or Graves’ disease (GD)] or nonautoimmune [nontoxic goiter (NTG) or papillary cancer (PC)] thyroid diseases. We found clear positivity of thyroid follicular cells for B7.1 in HT but not in GD, nor in nonautoimmune specimens (NTG, PC) using in situ analysis by alkaline phosphatase anti-alkaline phosphatase (APAAP) technique. Double immunostaining experiments in combination with an anti-human thyroglobulin antibody confirmed follicular B7.1 localization. On the contrary, no follicular B7.2 expression was observed in any specimen analyzed. These findings were confirmed by immunofluorescence flow cytometry on isolated follicular cells. The cytokines IL1beta and LPS were able to induce de novo B7.1 expression on cultured thyroid follicular cells. Intrathyroid T cells proved responsive to stimulation via the B7 ligand CD28, even in the absence of IL2. Moreover preliminary evidence was obtained for an inhibitory effect of anti-B7.1 mAb on T-cell proliferation in coculture with isolated thyroid follicular cells. It is conceivable that in HT, expression of B7.1 on follicular cells, together with MHC class II antigens and ICAM1, could provide a local costimulatory signal for T-lymphocyte differentiation toward the type 1 cytokine secretion pattern and maintenance of the autoimmune process.
Immunoprecipitation
Zhao, Y., et al (2019). "PD-L1:CD80 Cis-Heterodimer Triggers the Co-stimulatory Receptor CD28 While Repressing the Inhibitory PD-1 and CTLA-4 Pathways" Immunity 51(6): 1059-1073.e1059.
PubMed
Combined immunotherapy targeting the immune checkpoint receptors cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) and programmed cell death 1 (PD-1), or CTLA-4 and the PD-1 ligand (PD-L1) exhibits superior anti-tumor responses compared with single-agent therapy. Here, we examined the molecular basis for this synergy. Using reconstitution assays with fluorescence readouts, we found that PD-L1 and the CTLA-4 ligand CD80 heterodimerize in cis but not trans. Quantitative biochemistry and cell biology assays revealed that PD-L1:CD80 cis-heterodimerization inhibited both PD-L1:PD-1 and CD80:CTLA-4 interactions through distinct mechanisms but preserved the ability of CD80 to activate the T cell co-stimulatory receptor CD28. Furthermore, PD-L1 expression on antigen-presenting cells (APCs) prevented CTLA-4-mediated trans-endocytosis of CD80. Atezolizumab (anti-PD-L1), but not anti-PD-1, reduced cell surface expression of CD80 on APCs, and this effect was negated by co-blockade of CTLA-4 with ipilimumab (anti-CTLA-4). Thus, PD-L1 exerts an immunostimulatory effect by repressing the CTLA-4 axis; this has implications to the synergy of anti-PD-L1 and anti-CTLA-4 combination therapy.
in vitro T cell stimulation/activation
Blewett, M. M., et al (2016). "Chemical proteomic map of dimethyl fumarate-sensitive cysteines in primary human T cells" Sci Signal 9(445): rs10.
PubMed
Dimethyl fumarate (DMF) is an electrophilic drug that is used to treat autoimmune conditions, including multiple sclerosis and psoriasis. The mechanism of action of DMF is unclear but may involve the covalent modification of proteins or DMF serving as a prodrug that is converted to monomethyl fumarate (MMF). We found that DMF, but not MMF, blocked the activation of primary human and mouse T cells. Using a quantitative, site-specific chemical proteomic platform, we determined the DMF sensitivity of >2400 cysteine residues in human T cells. Cysteines sensitive to DMF, but not MMF, were identified in several proteins with established biochemical or genetic links to T cell function, including protein kinase Ctheta (PKCtheta). DMF blocked the association of PKCtheta with the costimulatory receptor CD28 by perturbing a CXXC motif in the C2 domain of this kinase. Mutation of these DMF-sensitive cysteines also impaired PKCtheta-CD28 interactions and T cell activation, designating the C2 domain of PKCtheta as a key functional, electrophile-sensing module important for T cell biology.
in vitro T cell stimulation/activation
Edwards, L. J., et al (2015). "Signal transducer and activator of transcription (STAT) 3 inhibition delays the onset of lupus nephritis in MRL/lpr mice" Clin Immunol 158(2): 221-230.
PubMed
The transcription factor STAT3 is overexpressed and hyperactivated in T cells from SLE patients. STAT3 plays a central role in T cell differentiation into Th17 and T follicular helper cells, two subsets that orchestrate autoimmune responses in SLE. Moreover, STAT3 is important in chemokine-mediated T cell migration. To better understand its role in SLE, we inhibited STAT3 in lupus-prone mice using the small molecule Stattic. Stattic-treated mice exhibited delayed onset of proteinuria (3 weeks later than controls), and had lower levels of anti-dsDNA antibodies and inflammatory cytokines. Inhibitor treatment reduced lymphadenopathy, resulted in a 3-fold decrease in total T cell number, and a 4-fold decrease in the numbers of T follicular helper cells. In vitro experiments showed that Stattic-treated T cells exhibited decreased proliferation and a decrease in ability to migrate to CXCL12. We propose that STAT3 inhibition represents a therapeutic target in SLE, particularly lupus nephritis.
Flow Cytometry
Leonard, J. A., et al (2011). "HIV-1 Nef disrupts intracellular trafficking of major histocompatibility complex class I, CD4, CD8, and CD28 by distinct pathways that share common elements" J Virol 85(14): 6867-6881.
PubMed
The Nef protein is an important HIV virulence factor that promotes the degradation of host proteins to augment virus production and facilitate immune evasion. The best-characterized targets of Nef are major histocompatibility complex class I (MHC-I) and CD4, but Nef also has been reported to target several other proteins, including CD8beta, CD28, CD80, CD86, and CD1d. To compare and contrast the effects of Nef on each protein, we constructed a panel of chimeric proteins in which the extracellular and transmembrane regions of the MHC-I allele HLA-A2 were fused to the cytoplasmic tails of CD4, CD28, CD8beta, CD80, CD86, and CD1d. We found that Nef coprecipitated with and disrupted the expression of molecules with cytoplasmic tails from MHC-I HLA-A2, CD4, CD8beta, and CD28, but Nef did not bind to or alter the expression of molecules with cytoplasmic tails from CD80, CD86, and CD1d. In addition, we used short interfering RNA (siRNA) knockdown and coprecipitation experiments to implicate AP-1 as a cellular cofactor for Nef in the downmodulation of both CD28 and CD8beta. The interaction with AP-1 required for CD28 and CD8beta differed from the AP-1 interaction required for MHC-I downmodulation in that it was mediated through the dileucine motif within Nef (LL(164,165)AA) and did not require the tyrosine binding pocket of the AP-1 mu subunit. In addition, we demonstrate a requirement for beta-COP as a cellular cofactor for Nef that was necessary for the degradation of targeted molecules HLA-A2, CD4, and CD8. These studies provide important new information on the similarities and differences with which Nef affects intracellular trafficking and help focus future research on the best potential pharmaceutical targets.
Immunoprecipitation
Zhao, Y., et al (2019). "PD-L1:CD80 Cis-Heterodimer Triggers the Co-stimulatory Receptor CD28 While Repressing the Inhibitory PD-1 and CTLA-4 Pathways" Immunity 51(6): 1059-1073.e1059.
PubMed
Combined immunotherapy targeting the immune checkpoint receptors cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) and programmed cell death 1 (PD-1), or CTLA-4 and the PD-1 ligand (PD-L1) exhibits superior anti-tumor responses compared with single-agent therapy. Here, we examined the molecular basis for this synergy. Using reconstitution assays with fluorescence readouts, we found that PD-L1 and the CTLA-4 ligand CD80 heterodimerize in cis but not trans. Quantitative biochemistry and cell biology assays revealed that PD-L1:CD80 cis-heterodimerization inhibited both PD-L1:PD-1 and CD80:CTLA-4 interactions through distinct mechanisms but preserved the ability of CD80 to activate the T cell co-stimulatory receptor CD28. Furthermore, PD-L1 expression on antigen-presenting cells (APCs) prevented CTLA-4-mediated trans-endocytosis of CD80. Atezolizumab (anti-PD-L1), but not anti-PD-1, reduced cell surface expression of CD80 on APCs, and this effect was negated by co-blockade of CTLA-4 with ipilimumab (anti-CTLA-4). Thus, PD-L1 exerts an immunostimulatory effect by repressing the CTLA-4 axis; this has implications to the synergy of anti-PD-L1 and anti-CTLA-4 combination therapy.
in vitro T cell stimulation/activation
Blewett, M. M., et al (2016). "Chemical proteomic map of dimethyl fumarate-sensitive cysteines in primary human T cells" Sci Signal 9(445): rs10.
PubMed
Dimethyl fumarate (DMF) is an electrophilic drug that is used to treat autoimmune conditions, including multiple sclerosis and psoriasis. The mechanism of action of DMF is unclear but may involve the covalent modification of proteins or DMF serving as a prodrug that is converted to monomethyl fumarate (MMF). We found that DMF, but not MMF, blocked the activation of primary human and mouse T cells. Using a quantitative, site-specific chemical proteomic platform, we determined the DMF sensitivity of >2400 cysteine residues in human T cells. Cysteines sensitive to DMF, but not MMF, were identified in several proteins with established biochemical or genetic links to T cell function, including protein kinase Ctheta (PKCtheta). DMF blocked the association of PKCtheta with the costimulatory receptor CD28 by perturbing a CXXC motif in the C2 domain of this kinase. Mutation of these DMF-sensitive cysteines also impaired PKCtheta-CD28 interactions and T cell activation, designating the C2 domain of PKCtheta as a key functional, electrophile-sensing module important for T cell biology.
in vitro T cell stimulation/activation
Edwards, L. J., et al (2015). "Signal transducer and activator of transcription (STAT) 3 inhibition delays the onset of lupus nephritis in MRL/lpr mice" Clin Immunol 158(2): 221-230.
PubMed
The transcription factor STAT3 is overexpressed and hyperactivated in T cells from SLE patients. STAT3 plays a central role in T cell differentiation into Th17 and T follicular helper cells, two subsets that orchestrate autoimmune responses in SLE. Moreover, STAT3 is important in chemokine-mediated T cell migration. To better understand its role in SLE, we inhibited STAT3 in lupus-prone mice using the small molecule Stattic. Stattic-treated mice exhibited delayed onset of proteinuria (3 weeks later than controls), and had lower levels of anti-dsDNA antibodies and inflammatory cytokines. Inhibitor treatment reduced lymphadenopathy, resulted in a 3-fold decrease in total T cell number, and a 4-fold decrease in the numbers of T follicular helper cells. In vitro experiments showed that Stattic-treated T cells exhibited decreased proliferation and a decrease in ability to migrate to CXCL12. We propose that STAT3 inhibition represents a therapeutic target in SLE, particularly lupus nephritis.
in vitro T cell stimulation/activation
Oh, Y. M., et al (2015). "Ndrg1 is a T-cell clonal anergy factor negatively regulated by CD28 costimulation and interleukin-2" Nat Commun 6: 8698.
PubMed
Induction of T-cell clonal anergy involves serial activation of transcription factors, including NFAT and Egr2/3. However, downstream effector mechanisms of these transcription factors are not fully understood yet. Here we identify Ndrg1 as an anergy factor induced by Egr2. Ndrg1 is upregulated by anergic signalling and maintained at high levels in resting anergic T cells. Overexpression of Ndrg1 mimics the anergic state and knockout of the gene prevents anergy induction. Interestingly, Ndrg1 is phosphorylated and degraded by CD28 signalling in a proteasome-dependent manner, explaining the costimulation dependence of anergy prevention. Similarly, IL-2 treatment of anergic T cells, under conditions that lead to the reversal of anergy, also induces Ndrg1 phosphorylation and degradation. Finally, older Ndrg1-deficient mice show T-cell hyperresponsiveness and Ndrg1-deficient T cells aggravate inducible autoimmune inflammation. Thus, Ndrg1 contributes to the maintenance of clonal anergy and inhibition of T-cell-mediated inflammation.
Flow Cytometry
Leonard, J. A., et al (2011). "HIV-1 Nef disrupts intracellular trafficking of major histocompatibility complex class I, CD4, CD8, and CD28 by distinct pathways that share common elements" J Virol 85(14): 6867-6881.
PubMed
The Nef protein is an important HIV virulence factor that promotes the degradation of host proteins to augment virus production and facilitate immune evasion. The best-characterized targets of Nef are major histocompatibility complex class I (MHC-I) and CD4, but Nef also has been reported to target several other proteins, including CD8beta, CD28, CD80, CD86, and CD1d. To compare and contrast the effects of Nef on each protein, we constructed a panel of chimeric proteins in which the extracellular and transmembrane regions of the MHC-I allele HLA-A2 were fused to the cytoplasmic tails of CD4, CD28, CD8beta, CD80, CD86, and CD1d. We found that Nef coprecipitated with and disrupted the expression of molecules with cytoplasmic tails from MHC-I HLA-A2, CD4, CD8beta, and CD28, but Nef did not bind to or alter the expression of molecules with cytoplasmic tails from CD80, CD86, and CD1d. In addition, we used short interfering RNA (siRNA) knockdown and coprecipitation experiments to implicate AP-1 as a cellular cofactor for Nef in the downmodulation of both CD28 and CD8beta. The interaction with AP-1 required for CD28 and CD8beta differed from the AP-1 interaction required for MHC-I downmodulation in that it was mediated through the dileucine motif within Nef (LL(164,165)AA) and did not require the tyrosine binding pocket of the AP-1 mu subunit. In addition, we demonstrate a requirement for beta-COP as a cellular cofactor for Nef that was necessary for the degradation of targeted molecules HLA-A2, CD4, and CD8. These studies provide important new information on the similarities and differences with which Nef affects intracellular trafficking and help focus future research on the best potential pharmaceutical targets.
Flow Cytometry
Rout, N., et al (2010). "Paucity of CD4+ natural killer T (NKT) lymphocytes in sooty mangabeys is associated with lack of NKT cell depletion after SIV infection" PLoS One 5(3): e9787.
PubMed
Lack of chronic immune activation in the presence of persistent viremia is a key feature that distinguishes nonpathogenic simian immunodeficiency virus (SIV) infection in natural hosts from pathogenic SIV and HIV infection. To elucidate novel mechanisms downmodulating immune activation in natural hosts of SIV infection, we investigated natural killer T (NKT) lymphocytes in sooty mangabeys. NKT lymphocytes are a potent immunoregulatory arm of the innate immune system that recognize glycolipid antigens presented on the nonpolymorphic MHC-class I-like CD1d molecules. In a cross-sectional analysis of 50 SIV-negative and 50 naturally SIV-infected sooty mangabeys, ligand alpha-galactosylceramide loaded CD1d tetramers co-staining with Valpha24-positive invariant NKT lymphocytes were detected at frequencies >or=0.002% of circulating T lymphocytes in approximately half of the animals. In contrast to published reports in Asian macaques, sooty mangabey NKT lymphocytes consisted of CD8(+) and CD4/CD8 double-negative T lymphocytes that were CXCR3-positive and CCR5-negative suggesting that they trafficked to sites of inflammation without being susceptible to SIV infection. Consistent with these findings, there was no difference in the frequency or phenotype of NKT lymphocytes between SIV-negative and SIV-infected sooty mangabeys. On stimulation with alpha-galactosylceramide loaded on human CD1d molecules, sooty mangabey NKT lymphocytes underwent degranulation and secreted IFN-gamma, TNF-alpha, IL-2, IL-13, and IL-10, indicating the presence of both effector and immunoregulatory functional capabilities. The unique absence of CD4(+) NKT lymphocytes in sooty mangabeys, combined with their IL-10 cytokine-secreting ability and preservation following SIV infection, raises the possibility that NKT lymphocytes might play a role in downmodulating immune activation in SIV-infected sooty mangabeys.
Immunohistochemistry (frozen)
Tazi, A., et al (1999). "Evidence that Langerhans cells in adult pulmonary Langerhans cell histiocytosis are mature dendritic cells: importance of the cytokine microenvironment" J Immunol 163(6): 3511-3515.
PubMed
Because Langerhans cells (LC) in peripheral tissues are generally “immature” cells with poor lymphostimulatory activity, the contribution of immune responses initiated by LC to the pathogenesis of pulmonary LC histiocytosis (LCH) has been uncertain. In this study we demonstrate that LC accumulating in LCH granulomas are phenotypically similar to mature lymphostimulatory dendritic cells present in lymphoid organs. LC in LCH granulomas intensely expressed B7-1 and B7-2 molecules, whereas normal pulmonary LC and LC accumulating in other pathologic lung disorders did not express these costimulatory molecules. The presence of B7+ LC in LCH granulomas was associated with the expression in these lesions, but not at other sites in the lung, of a unique profile of cytokines (presence of GM-CSF, TNF-alpha, and IL-1beta and the absence of IL-10) that is known to promote the in vitro differentiation of LC into cells expressing a lymphostimulatory phenotype. Finally, LCH granulomas were the only site where CD154-positive T cells could be identified in close contact with LC intensely expressing CD40 Ags. Taken together, these results strongly support the idea that an abnormal immune response initiated by LC may participate in the pathogenesis of pulmonary LCH, and suggest that therapeutic strategies aimed at modifying the lymphostimulatory phenotype of LC may be useful in the treatment of this disorder.
Immunohistochemistry (frozen)
Battifora, M., et al (1998). "B7.1 costimulatory molecule is expressed on thyroid follicular cells in Hashimoto’s thyroiditis, but not in Graves’ disease" J Clin Endocrinol Metab 83(11): 4130-4139.
PubMed
The molecules of the B7 family play a major role in T-lymphocyte costimulation through interaction with their counterreceptors CD28 and CTLA4. In the present study, we analyzed the possible expression of B7 molecules on surgically removed thyroid tissue of patients with autoimmune [Hashimoto’s thyroiditis (HT) or Graves’ disease (GD)] or nonautoimmune [nontoxic goiter (NTG) or papillary cancer (PC)] thyroid diseases. We found clear positivity of thyroid follicular cells for B7.1 in HT but not in GD, nor in nonautoimmune specimens (NTG, PC) using in situ analysis by alkaline phosphatase anti-alkaline phosphatase (APAAP) technique. Double immunostaining experiments in combination with an anti-human thyroglobulin antibody confirmed follicular B7.1 localization. On the contrary, no follicular B7.2 expression was observed in any specimen analyzed. These findings were confirmed by immunofluorescence flow cytometry on isolated follicular cells. The cytokines IL1beta and LPS were able to induce de novo B7.1 expression on cultured thyroid follicular cells. Intrathyroid T cells proved responsive to stimulation via the B7 ligand CD28, even in the absence of IL2. Moreover preliminary evidence was obtained for an inhibitory effect of anti-B7.1 mAb on T-cell proliferation in coculture with isolated thyroid follicular cells. It is conceivable that in HT, expression of B7.1 on follicular cells, together with MHC class II antigens and ICAM1, could provide a local costimulatory signal for T-lymphocyte differentiation toward the type 1 cytokine secretion pattern and maintenance of the autoimmune process.